Achieving Whole Health – A New Approach for Veterans and the Nation
EDITOR’S NOTE: PCC President Harold Kudler, MD, is involved in national and international efforts to improve health using talk therapy and psychoanalytically informed therapy whenever possible. He is too humble to share a c.v., but if you Google him, you will find many publications, Congressional testimonies, podcasts, videos, and more. He recently helped co-author a report by the National Academies of Science, Engineering, and Medicine recommending a system of whole health care as described in the article below. Dr. Kudler says, “I look forward to discussing our findings and recommendations with you and ask that you join me on how to fill gaps and create processes to accelerate the transformation to whole health care for all people.”
A Message from Harold Kudler

The National Academies recommendations for implementing, scaling, and spreading a national system of whole healthcare offer the potential to improve health and well-being and advance effective, efficient, and equitable care delivery.
Whole health is physical, behavioral, spiritual, and socioeconomic well-being as defined by individuals, families, and communities. Whole Health care is an interprofessional, team-based approach anchored in trusted relationships to promote well-being, prevent disease, and restore health. It aligns with a person’s life mission, aspirations, and purpose. It changes the healthcare conversation from “What’s wrong with you?” to “What matters to you?”
The National Academies of Sciences, Engineering, and Medicine’s recommendations for implementing, scaling, and spreading a national system of whole healthcare offer the potential to improve health and well-being and advance effective, efficient, and equitable care delivery. I look forward to discussing our findings and recommendations with you and ask that you join me in sharing our report as widely as possible.
Whole health is physical, behavioral, spiritual, and socioeconomic well-being as defined by individuals, families, and communities. Whole Health care is an interprofessional, team-based approach anchored in trusted relationships to promote well-being, prevent disease, and restore health. It aligns with a person’s life mission, aspirations, and purpose. It changes the healthcare conversation from “What’s wrong with you?” to “What matters to you?”
The current medical care infrastructure in the United States, with its orientation toward disease treatment and the dominant fee-for-service payment model, has demonstrated that it is incapable of treating people fairly and systematically, let alone of promoting well-being and preventing the onset of disease. New goals and a systematic reorientation of resources and activities are needed. For these reasons, I was glad to serve as a member of a multidisciplinary committee (and as its only psychiatrist and psychoanalytically oriented clinician) to examine the potential for improving health outcomes through a whole health model. The Department of Veterans Affairs (VA), the Samueli Foundation, and the Whole Health Institute commissioned our report through the National Academies of Sciences, Engineering, and Medicine. Our charge was to provide guidance on how to accelerate the transformation to whole health care for veterans and all Americans.
From the beginning, I was aware of a special resonance between Whole Health and the person-centered nature of psychoanalytic theory and practice which values what comes from the patient rather than what the clinician can detect, pronounce, or act upon. Our report was released on February 15 and can be found here.
Our 18 committee members studied care systems worldwide that were working to achieve whole health. We also considered evidence from three specially commissioned papers about patient-centeredness and reviewed data from the Department of Veterans Affairs (VA) Whole Health Initiative. We conducted a literature review that included more than 5000 articles.
Our key findings include:
- Having whole health is fundamentally different from being healthy in a biomedical model.
- Health must be defined by individuals, families, and communities in collaboration with an interprofessional, team-based approach anchored in trusted longitudinal relationships which promote resilience, prevent disease, and restore health.
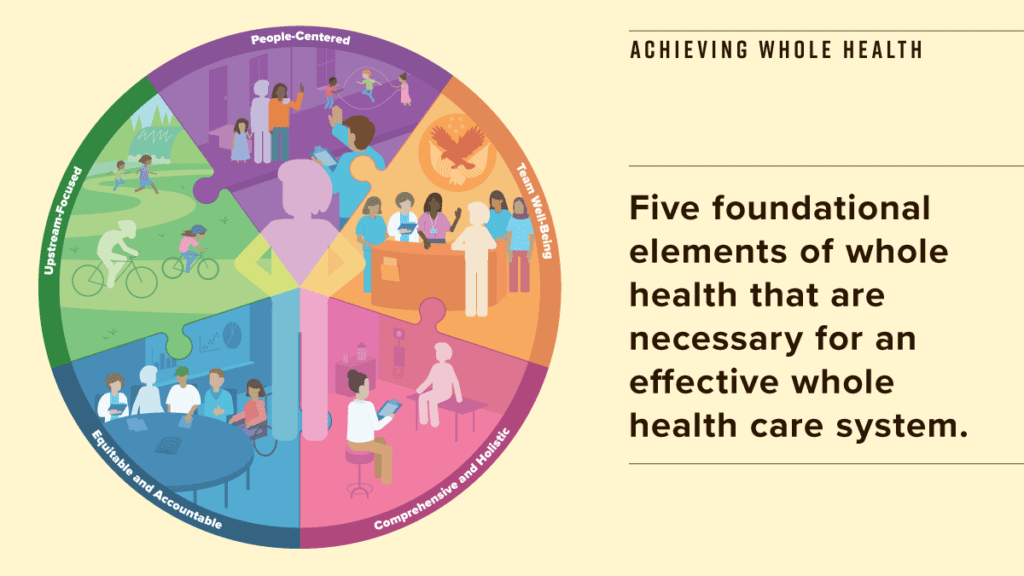
- Whole health is people-centered, comprehensive and holistic, upstream-focused, equitable and accountable, and ensures team well-being.
- Achieving whole health starts with understanding what matters to people and then building the environment, resources, and support to help people and communities achieve their life goals.
- This perspective transcends the disease-reactive approach which dominates U.S. health care by proactively addressing structural and social determinants of health to focus on wellness rather than sickness.
Scaling and spreading whole health to all veterans and all individuals, families, and communities will require a seismic shift in how the U.S. conceives, delivers, and pays for health care. It also requires fundamental realignment of community, state, and federal social services and population health programs with current clinical operations to improve health outcomes while lowering costs.